If you’re here, chances are you’ve been struggling with unexplained pain, frustrating doctor visits, and maybe even feeling dismissed when you bring up your symptoms.
Living with undiagnosed endometriosis is exhausting—physically, mentally, and emotionally. The pain can be debilitating, making it hard to work, maintain relationships, or even get through daily tasks. Meanwhile, the constant dismissal from doctors can leave you questioning yourself, wondering if you’re overreacting, when deep down, you know something is wrong. Many people go years, sometimes over a decade, before they finally get answers.
This guide will help you understand when to seek a specialist and how to advocate for yourself, so you can finally get the care you need.
Choosing the Right Specialist
General Gynecologists
Endometriosis is a complex disease that requires specialized care. Unfortunately, most primary care doctors and even general OB/GYNs don’t have extensive training in diagnosing and treating it. They may only offer symptom management—such as birth control, painkillers, or hormone therapy—rather than addressing the root cause of your condition. The downside? The longer endometriosis is left untreated, the more damage it can cause. Seeking a specialist early can mean a better quality of life in the long run.
Fertility Specialists
Fertility specialists or reproductive endocrinologists (REs) play an important role in the care of many people with endometriosis, particularly those struggling to conceive. However, it’s important to understand that fertility specialists focus on assisted reproductive technology (ART), such as IVF, and do not typically perform excision surgery unless they have received extensive additional training in this area. If you are trying to conceive and have endometriosis, working with both a fertility specialist and an excision specialist can provide the best approach to managing your condition and improving your chances of a successful pregnancy.
Watch On-Demand: IVF vs. Endometriosis Surgery – The Role of Office Testing & Collaborative Planning
Endometriosis Specialists
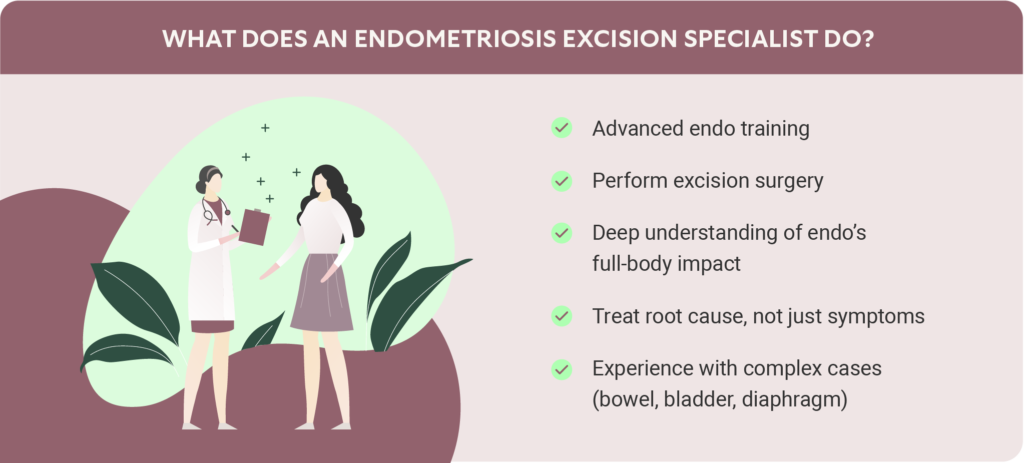
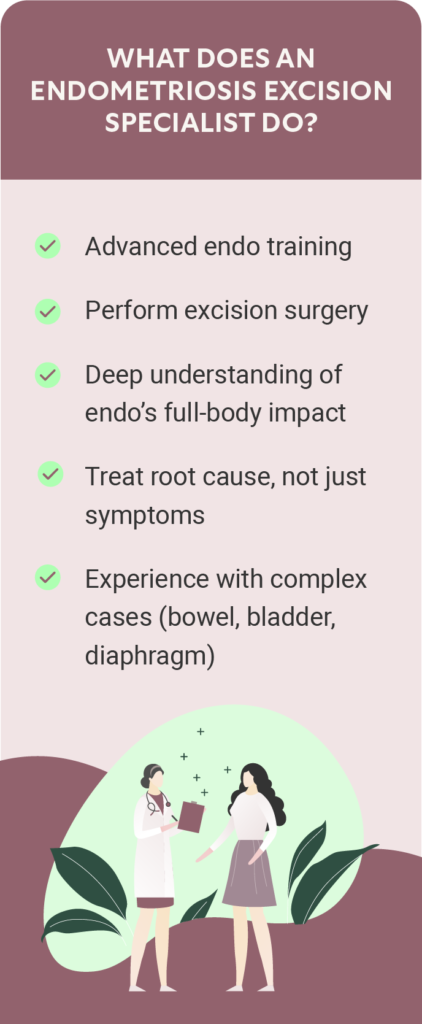
A true endometriosis excision specialist is a gynecologist with advanced training in recognizing, diagnosing, and surgically treating endometriosis. Unlike general OB/GYN surgeons, these specialists:
- Perform excision surgery, the gold standard for removing endometriosis tissue, rather than just burning or suppressing it.
- Have a deeper understanding of how endo affects the body, including the bowel, bladder, diaphragm, and even the lungs.
- Offer a higher chance of reducing pain, preserving fertility, and lowering recurrence rates compared to non-specialist treatments.
Don’t be afraid to travel for the right specialist. Endometriosis is a serious disease, and you deserve a doctor who treats your condition properly. If you’re not comfortable with the care your doctor is providing, trust your gut. Consider a virtual consultation with an out-of-town doctor if there aren’t any specialists near you.
When to Seek Out a Specialist
You might be wondering, “Is it time for me to see a specialist?” If any of the following apply to you, the answer is yes.
1. You Have Endo Symptoms and Risk Factors
Endometriosis symptoms vary, but common signs include:
- Chronic pelvic pain
- Painful periods (dysmenorrhea)
- Pain with sex
- Bowel or urinary issues, especially during your cycle
- Fatigue
- Unexplained infertility
Note: Up to 80% of women with pelvic pain and 50% of women with infertility have endometriosis. If you have one or both of these issues and have been dismissed by your doctor, seek a second opinion.
In addition to ongoing physical symptoms, certain risk factors can increase the likelihood of having endometriosis, including:
- Family history (mother, aunt, or sister with endo)
- Early first period (before age 11)
- Short menstrual cycles (less than 27 days)
- Never having been pregnant
- Low BMI
If you have symptoms that interfere with your daily life and aren’t getting answers, it’s time to seek a specialist.
2. Your Doctor’s Treatment Plan Focuses Only on Symptoms
If your doctor has only offered temporary fixes like birth control, pain medication, or hormone therapy without discussing surgical options, they may not be the right provider for your case. Additionally, many gynecological surgeons only offer ablation surgery, where endometriosis is burned off of internal organs and tissues. Endometriosis specialists can provide excision surgery, which is the most effective treatment for actually removing endometriosis tissue and providing long-term relief.
3. You Have Been Diagnosed with Advanced Endometriosis
Video: True or False – Vaginal Endometriosis Isn’t a Big Deal?
A diagnosis of stage III or stage IV endometriosis often means the disease has deeply infiltrated areas like the vagina, rectum, bladder, or bowels. These cases require specialized surgical care to prevent complications. Delaying care for advanced endo can lead to more invasive surgeries and a higher risk of long-term organ damage.
Symptoms you shouldn’t ignore include:
- Rectal bleeding during menstruation
- Severe constipation or difficulty passing stool
- Persistent urinary issues
- Painful bowel movements or urination
4. Imaging Has Shown Endometriomas
Endometriomas—also called “chocolate cysts”—are cysts filled with old blood that form on the ovaries. If left untreated, they can rupture, spread endometriosis further, and cause painful adhesions that make future surgeries more difficult. Laparoscopic surgery is the only definitive way to diagnose endometriosis, but if an ultrasound or MRI has detected an endometrioma, a specialist should evaluate your case as soon as possible.
5. You’ve Had Unsuccessful Surgeries for Persistent Symptoms
If you’ve already had one or more pelvic surgeries but your symptoms haven’t improved (or have gotten worse), it’s a red flag that your previous surgeon may not have removed all of the endometriosis tissue. Symptoms that warrant seeing a specialist include:
- Severe pelvic or abdominal pain despite past surgery
- Lung issues (such as lung collapse or shortness of breath during your period)
- Bowel or urinary problems that didn’t resolve after previous treatment
Additionally, if you’ve had any abdominal surgeries in the past (even unrelated to endo, such as a C-section birth), scar tissue from those surgeries can sometimes make endometriosis worse. A specialist can assess whether this is affecting your case.
How to Advocate for Yourself with Your Doctor
Depending on your insurance policy, you may need a referral from your doctor to see an endometriosis specialist, so being firm and informed can help you get the care you deserve. If you suspect you have endometriosis and want to see a specialist, but your doctor isn’t listening, here are some ways to advocate for yourself, including specific things you can say during your appointment.
- Be direct about your symptoms.
What to say: “My symptoms are affecting my quality of life. I am struggling to function at work/school/home because of my pain.”
- Ask about their expertise.
What to say: “What training and experience do you have in endometriosis excision surgery?”
Note: Even with gynecological training, traditional medical school does not provide doctors with endometriosis expertise. Endometriosis specialists complete post-residency fellowships focused on diagnosing and surgically managing endometriosis.
- Push for a referral.
What to say: “I would like a referral to an endometriosis specialist.”
If they refuse, say, “Please note in my medical chart that I asked for a specialist referral and you declined.” This may nudge the doctor to provide the referral.
Get more tips in our endometriosis patient advocacy guide.
ESSE Care Is Here to Help
Finding the right specialist can be overwhelming, but you don’t have to navigate this alone. At ESSE Care, our experienced team of endometriosis specialists can review your case, provide second (or third or fourth) opinions, and help you take the next step toward relief.
If you’re tired of being dismissed or misdiagnosed, it’s time to take control of your health. Schedule a consultation with ESSE Care today and get the answers you deserve.












