For people living with endometriosis, an endometrioma can be especially painful and damaging. While often misunderstood as benign, stable, or even reversible, these cysts can cause severe complications and threaten future fertility. Surgical intervention, when timed and executed well, can prevent long-term damage and improve a patient’s quality of life.
Far too often, patients are dismissed without accurate information. At ESSE Care, we’ve seen what happens when endometriomas are left to grow without proper treatment: real harm from ruptures and adhesions that could have been prevented.
What Is an Endometrioma?
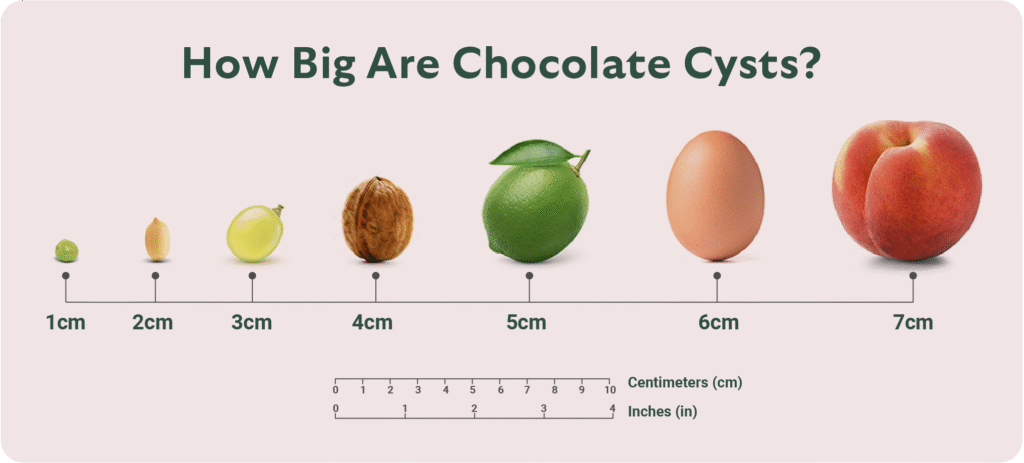
An endometrioma is a type of ovarian cyst commonly associated with endometriosis. Often called “chocolate cysts,” they’re filled with thick, dark fluid and can become large, painful, and destructive over time. Unlike functional ovarian cysts, endometriomas don’t go away on their own and typically don’t respond well to hormonal suppression. In many cases, surgery is the most effective and necessary treatment.
The presence of endometriomas is a sign of deep disease. Over time, endometriomas can grow, press on nearby organs, and even rupture. When they do, their contents can cause inflammation and scar tissue throughout the pelvis. That’s why they often come with pain and fertility challenges that lead patients to seek skilled surgical care. potentially allowing their condition to worsen. In a recent surgery, Dr. Goldstein treated a patient who had been incorrectly informed that her endometrioma was only 3–4 cm. However, by the time she came to surgery, the cyst had grown to 6.5 cm and had already ruptured, leaking its contents into surrounding tissues.

ESSE Care Case Study: Endometrioma Rupture and Cyst Splatter
Video: Endometrioma Myths: Yes, They Can Rupture
We often see patients who have been told for years that their endometrioma is smaller than it turns out to be, and not to worry because endometriomas don’t rupture. Unfortunately, this isn’t always true.
In the case of one ESSE Care patient, she had delayed surgery for an endometrioma based on this kind of advice. Previous doctors told her she had a 3-4 centimeter cyst, but surgery revealed a 6.5-centimeter ruptured cyst that spilled inflammatory contents into the pelvis. The result was dense adhesions to the bowel, bladder, uterus, and other pelvic organs. What could have been a straightforward surgery progressed to a complex case requiring extensive excision.
Fluid from a ruptured cyst can splatter and harden onto pelvic structures. It often doesn’t show up on scans, but it can cause pain, inflammation, and long-term complications.
Endometrioma Diagnosis and Pre-Operative Plan
Before surgery, we use imaging like ultrasounds and MRIs to locate the cyst and assess the extent of disease. We take a thorough history and ask about pain, symptoms, fertility goals, and your journey thus far—because those details shape everything we do.
At ESSE Care, every surgery is tailored to meet individual needs. We plan to remove what’s visible, but also address what may be hiding beneath the surface. We prepare for the unexpected, because with endometriosis, there’s almost always more going on than meets the eye.
Inside the OR: Endometrioma Surgery Breakdown
Video: Cyst Splatter and Adhesions: The Urgent Case for Early Endometrioma Surgery
Endometrioma surgery is usually done laparoscopically—minimally invasive, using small incisions and a camera. Once inside, we carefully inspect the pelvis and assess what’s really happening.
Adhesions or scar tissue are often the first obstacle causing organs to stick together. Careful dissection is required to free the ovaries and surrounding structures. Once we locate the cyst, we work to remove it from the ovary without damaging the surrounding healthy ovarian tissue—a critical step in preserving fertility.
In more severe cases, like the one mentioned above, we find extensive adhesions that require meticulous excision and advanced reconstructive techniques. Using laparoscopic tools, we remove leftover cyst material and endometriosis lesions from the pelvic walls, bowel, bladder, and uterus, restoring normal anatomy as much as possible.
A key part of every endometrioma surgery at ESSE Care is meticulous ovarian reconstruction. When we remove a cyst from the ovary, we take extra care to avoid damaging healthy tissue. Instead of using heat or cautery to stop bleeding, we suture the ovary by hand. This reduces the risk of harming ovarian follicles, which are essential for hormone health and fertility.
Suturing also plays a critical role in preventing additional adhesions, which often form where there’s uncontrolled bleeding. By controlling bleeding through careful stitching and restoring the ovary’s natural shape, we reduce the risk of future complications like bowel sticking to the ovary, which can lead to serious long-term issues, such as potential bowel surgery.
Our approach is all about protecting what matters most: your health, your fertility, and your future. Every stitch, every step is done with that goal in mind.
What to Expect After Endometrioma Surgery
Patients typically recover well from laparoscopic endometrioma surgery. For many, surgery is the first time their pain is taken seriously, and that emotional relief matters, too.
After surgery, patients can walk and move gently as part of the healing process. Full recovery can take up to six weeks. ESSE Care patients see us within the first week or so after surgery, and again once pathology results come back (typically about two weeks later). These visits are important touchpoints to assess healing and discuss what’s next—whether that’s symptom management, fertility planning, or both.
Hormonal therapy is often recommended after surgery to help prevent recurrence. For those trying to conceive, fertility counseling is part of the post-op care plan. At ESSE Care, we take a whole-body approach to healing, ensuring your mind, body, and spirit are supported throughout your journey.
Why This Matters
Too many people are told to “wait and see” with endometriomas—without being told what that waiting might cost. Online misinformation may even lead patients to believe that they can shrink endometriomas on their own through diet and exercise, which isn’t true. Lifestyle interventions paired with hormonal therapy can improve symptoms, but the underlying endometrioma remains, and it can potentially grow and leak over time.
Ruptures and splatter do happen. And when they do, it’s not just the cyst you’re dealing with anymore. It’s inflammation, widespread endometriosis lesions, and damage to the organs that support your fertility and quality of life.
Here are the key takeaways from this case:
- Endometriomas do not disappear on their own. Most often, these cysts grow larger with each menstrual cycle and worsen symptoms.
- Endometriomas can rupture. The leaked fluid can cause serious complications by adhering to nearby organs. The contents can spread, forming new lesions and adhesions that make future surgeries more difficult.
- Early, expert surgery can prevent further damage and relieve symptoms. It’s essential to have accurate diagnoses and timely surgical intervention to be proactive.
You deserve real answers, not dismissal. And if you’ve already had a rupture or been told your cyst is “nothing,” know this: There’s still a path forward, and we’re here to help you walk it.
Dr. Goldstein’s Final Thoughts
“So many of my patients come to me after years of being told they’re overreacting. It’s frustrating to meet patients who were told not to worry, only to see firsthand the damage a ruptured endometrioma can do. But I also see how powerful the right treatment can be. That’s why I’m passionate about educating patients—so they can make empowered decisions about their care.” – Dr. Karli Provost Goldstein
You deserve doctors who believe you. If you’re unsatisfied with the treatment you’ve received for your endometriosis, ESSE Care is here to provide expert care and honest answers.
Reach out today for a case review and to learn more about our compassionate approach to patient care.