Dr. Emily Sbiroli on Emergency Care, Endometriosis, and Being Taken Seriously in the ER
For many patients living with endometriosis, the ER is one of the first—and most painful—stops in their care journey. Severe pelvic pain, ruptured cysts, and flares can bring you to an emergency department or urgent care quickly. But what happens when nothing shows up on imaging, and your pain is dismissed as “just a cyst”?
We know that emergency care is often where endometriosis patients first feel invisible. That’s why we work with providers who are changing the narrative from inside the system—physicians who understand what it’s like to live with endo and who advocate for better care across all settings.
We’re proud to work alongside Dr. Emily Sbiroli, a board-certified emergency physician in San Diego and endometriosis patient herself. She joined Dr. Karli Provost Goldstein and Gina Carloto for our Ruptured Cyst vs. Endometriosis Flare webinar to answer the most pressing questions our patients are asking—and to help decode what the ER can and can’t do when the pain becomes urgent.
About Dr. Emily Sbiroli
Dr. Sbiroli brings a rare dual perspective—as both an ER doctor and a patient living with endometriosis. After 7 years of unexplained infertility and decades of painful cycles, she was diagnosed with endo and underwent excision surgery in 2025. Her personal and professional experiences drive her mission to reform how emergency care treats invisible illnesses.
Advocate for endometriosis awareness and diagnostic equity in the ER:
- Board-certified emergency physician based in San Diego
- Specialist in emergency care for diverse and underserved populations
- Diagnosed with silent endometriosis after years of misdiagnosis
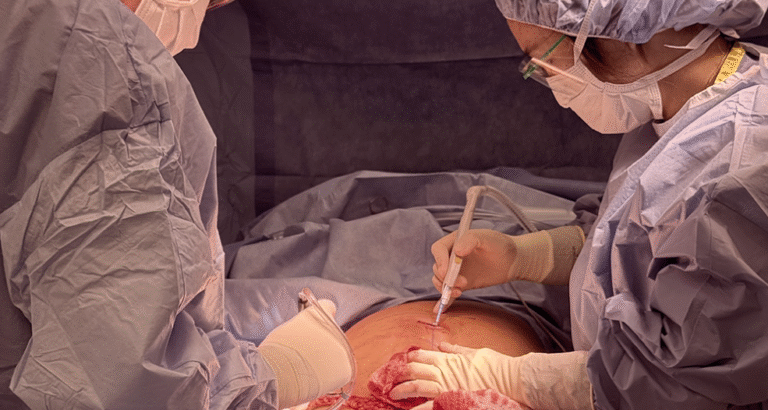
- Experienced excision surgery and postoperative recovery firsthand
What our patients are asking—Dr. Sbiroli and Dr. Goldstein answer your top ER questions
What is the ER designed to do?
Dr. Sbiroli’s Answer: The ER is built to rule out imminently life or limb-threatening conditions—like ectopic pregnancy, ovarian torsion, bowel obstruction, dangerous infections, or hemorrhage. Since the diagnosis of endometriosis often requires extensive lab work testing, advanced imaging, or confirmatory surgery, it is often missed in emergency departments due to a lack of resources. Simply put, the ER is not designed to diagnose endometriosis or create long-term care plans officially and patients are often frustrated with this. But it can help manage severe pain and identify emergencies that need immediate attention.
What kinds of tests will the ER run if I show up with pelvic pain?
Dr. Sbiroli’s Answer: The ER doctor wants to know what else is potentially going on besides endometriosis, and your testing and treatment plan will reflect that. Expect a pregnancy test, urinalysis, basic bloodwork, and an ultrasound or CT scan, depending on where your pain is. The ER doctor may also want to perform a pelvic exam to evaluate your cervix and ovaries. These all help the ER doctor check for infections, internal bleeding, or other surgical emergencies. But endometriosis—especially deep disease—often won’t appear on these tests. The vast majority of ER’s do not have hormone testing or MRI’s specific for endometriosis. This is mostly because these tests often require outside labs to run them that take days to come back, which would not be helpful when we need answers immediately in the ER, and MRI’s are reserved for life-threatening emergencies such as strokes or spinal cord injuries. Many emergency departments may also not have a gynecologist on call to evaluate you in the ER. This lack of resources can often leave endometriosis patients feeling unsatisfied or frustrated with their care in the emergency department.
What do ovarian cysts look like on imaging?
Dr. Sbiroli’s Answer: Simple cysts are fluid-filled and usually harmless. Hemorrhagic cysts may appear complex due to bleeding inside the cyst. Endometriomas (associated with endometriosis) have a distinct ground-glass appearance—but even they can be categorized as just a general ovarian cyst and not be identified as specifically an endometrioma, especially in a busy ER setting.
What if everything looks “normal” in the ER, but I’m still in pain?
Dr. Sbiroli’s Answer: You’re not imagining it. A normal scan or bloodwork doesn’t mean your pain isn’t real. It simply means that you do not need to be admitted to the hospital or have an imminently life-threatening emergency at the time of your visit. The best next step would be to follow up with a specialist who understands how endometriosis presents and can perform a deeper investigation with focused, specialized care.
When should I go to the ER for pelvic pain?
Dr. Sbiroli’s Answer: If your pain is sharp, sudden, and severe—especially with vomiting, fainting, heavy bleeding, or changes in bowel/bladder function—go in. A good rule of thumb is that if your pain feels different in any way from your usual pain, or if you cannot eat, drink, use the bathroom, or walk normally—go to the nearest emergency department. Safety first. Don’t wait for it to become an emergency.
How can I make sure I’m taken seriously in the ER?
Dr. Sbiroli’s Answer: Be specific. Say, “This is not my usual pain,” or “I have a history of ovarian cysts.” Bring documentation of any previous diagnoses or surgeries if you can. You can also say: “I know this may not give me long-term answers. I’m here for pain control and to rule out rupture or torsion.” You can also ask, “How do you recommend I follow up and with whom?” At the same time, you can also tell them what you don’t want. For example, if you are familiar with your pain and need help managing it, you can tell them you don’t want more CTs, ultrasounds, or pelvic exams. The ball is in your court.
Video: Endometriosis Was on the Scan—But Still Missed in the ER
Why Dr. Sbiroli is a trusted voice at ESSE
At ESSE, we don’t believe care should end when you leave the ER. Too many patients walk out without a diagnosis, a plan, or even validation, without really understanding why or what to do next. Dr. Sbiroli is helping to change that.
She brings empathy, clarity, and honesty to a space that often lacks all three. And she shows patients how to protect themselves—not just physically but emotionally.
Together, we’re building bridges between emergency care and specialist care—so no one has to navigate pelvic pain alone or unheard.