If you’ve been told you have Stage 1 endometriosis—or if you suspect you might—it’s easy to feel dismissed. Maybe a doctor implied it’s “just a little bit of endo” or said your symptoms couldn’t possibly be that bad at this stage. We’re here to tell you: Stage 1 doesn’t mean your pain isn’t real. It doesn’t mean you’re overreacting. And it doesn’t mean you don’t deserve relief.
Let’s take a closer look at what Stage 1 endometriosis is, how it’s diagnosed, symptoms, and next steps.
What Is the Endometriosis Staging System?
The American Society for Reproductive Medicine (ASRM) classifies endometriosis into four stages: Stage 1 (minimal), Stage 2 (mild), Stage 3 (moderate), and Stage 4 (severe). This system is based on a visual scoring system observed during surgery, based on location, amount, depth, and size of endometrial implants, as well as the presence of scar tissue (adhesions) or ovarian endometriomas (sometimes called “chocolate cysts”).
But here’s the part that matters most:
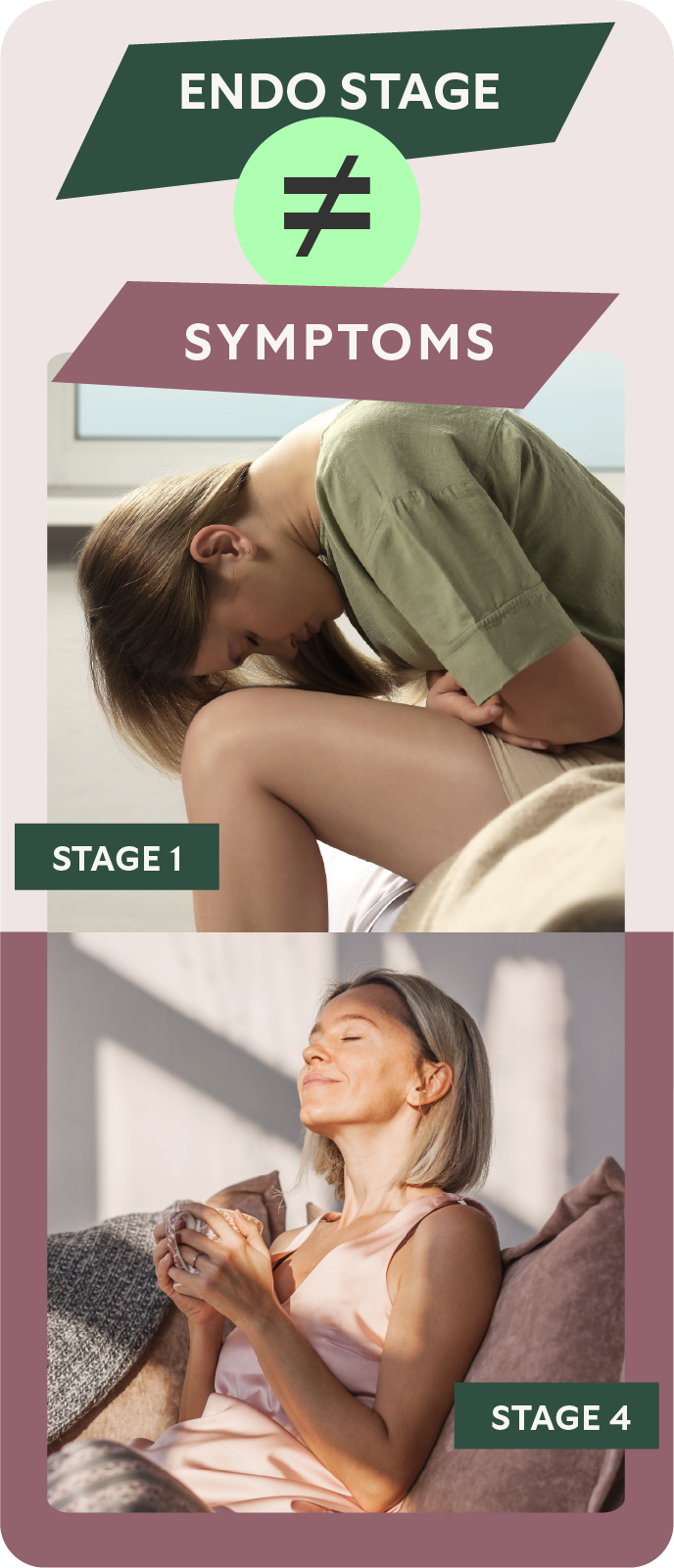
Staging is about what a surgeon sees—not what you feel.
That’s why someone with Stage 1 disease can experience debilitating pain, while someone with Stage 4 may have no symptoms at all. The staging system can be helpful for guiding treatment decisions, but it doesn’t define the impact endometriosis has on your life.

What Does Stage 1 Endometriosis Look Like?
Stage 1 is considered the “minimal” stage of endometriosis, and is typically characterized by:
- A few shallow, superficial implants (also called lesions)
- No significant scarring or adhesions
- No large ovarian cysts or structural damage
These implants may appear as clear, white, brown, or black spots on the surfaces of pelvic organs like the ovaries, fallopian tubes, bladder, or uterine ligaments.
Again, “minimal” describes the size and number of visible lesions, not the severity of symptoms.
Stage 1 Endometriosis Symptoms
It’s a frustrating truth: there is no correlation between the stage of endometriosis and its symptoms. Even the smallest lesions can trigger chronic inflammation and nerve sensitization, leading to symptoms that disrupt your daily life.
Common symptoms of Stage 1 endometriosis are similar to other stages:
- Painful, heavy periods
- Painful intercourse
- Pelvic pain, sometimes radiating to the back or thighs
- Pain with bowel movements
- Digestive issues (diarrhea, constipation, bloating, or nausea)
- Fatigue
Can Stage 1 endometriosis cause pain?
Absolutely. Even “minimal” disease can cause significant pain. Never let a doctor dismiss your symptoms just because of your stage.
If you’re in pain, you deserve answers—and options.
Can Stage 1 endometriosis affect fertility?
Yes, although it’s generally less likely to impair fertility than more advanced stages. Still, early-stage lesions can interfere with egg quality, fallopian tube function, or create inflammation that affects implantation.
How Is Stage 1 Endometriosis Diagnosed?
The only way to definitively diagnose endometriosis—at any stage—is through laparoscopic surgery, where a doctor uses a small camera to look inside your pelvis and take tissue samples for confirmation.
But getting to that point often takes years. Many people are misdiagnosed or dismissed. Imaging like ultrasounds or MRIs often appear normal, especially with Stage 1 disease, because small lesions are hard to detect without surgery.
If you’ve ruled out other conditions and your symptoms persist, a knowledgeable doctor may suspect endometriosis and recommend either symptom treatment (like hormonal therapy) or surgical evaluation.
Note: Not all gynecologic surgeons are trained to recognize and treat endometriosis effectively. Consider consulting an endometriosis excision specialist—someone with specialized expertise in identifying even the most hidden forms of the disease.
Stage 1 Endometriosis Treatments
There is no universal approach to treating endometriosis, especially in its early stages. The right treatment plan depends on your symptoms, goals, and preferences.
Common treatment options include:
- Hormonal therapies (birth control pills, progestins, GnRH medications): These can help suppress the hormonal cycles that feed endometrial tissue growth. They don’t remove lesions, but they may reduce symptoms.
- Excision surgery: A specialist can remove endometriosis lesions at the root, rather than just burning or cauterizing the surface. This can be especially effective for symptom relief and preserving fertility.
- Pain management and lifestyle support: Anti-inflammatory medications, pelvic floor therapy, dietary modifications, and mental health support can all play a role in improving overall well-being.
Remember; you have the power to say no and seek other care if what a doctor suggests isn’t aligned with your goals.
The Importance of Timely Endometriosis Surgery
Video: The Importance of Timely Endometriosis Surgery
Early intervention and the right timing of endometriosis surgery are crucial. By addressing the disease in its early stages, excision surgery can help you avoid the more complicated, high-risk scenarios seen with stage 4 endometriosis. Delaying surgery until endometriosis is in an advanced stage, especially when fertility is a concern, can complicate both the surgery and your future reproductive options. If you’re in your late twenties or early thirties, timely excision can offer more options for fertility preservation and a potentially pain-free life.
Need Help Finding Answers?
Too many patients with Stage 1 endo are told they should feel “lucky”—that it’s not bad enough to treat, or not serious enough to cause their symptoms.
At ESSE Care, we see it differently. If endometriosis is interfering with your ability to work or function, your relationships, or simply your peace of mind, that matters. You deserve to be heard, to be believed, and to explore all the options available to help you feel like yourself again.
The endometriosis specialists at ESSE Care prioritize compassionate care and expert diagnosis. Contact us to learn more or schedule a consultation.