Understanding Pelvic Pain: A Conversation with ESSE, Emergency Medicine, and Patient Advocacy
In this session of The Endo Exchange, Dr. Karli Provost Goldstein of ESSE Care was joined by Dr. Emily Sbiroli—a board-certified emergency medicine physician and endometriosis patient—and Gina Carloto, advocate, former Miss Connecticut, and founder of The Grace Collective, an organization dedicated to health advocacy and storytelling. Together, they unpacked a common yet misunderstood experience: what to do when pelvic pain sends you to the ER and how to tell the difference between a ruptured cyst, an endo flare, or a true emergency.
The session provided a clear and compassionate breakdown of how emergency care works, where it falls short, and what patients can do to protect themselves in high-stress medical settings.
Here are the top five takeaways from the conversation:
1. The ER rules out immediate threats—not chronic illness
Dr. Sbiroli explained that emergency departments are designed to identify and treat life-threatening conditions. They are not set up to diagnose chronic diseases like endometriosis. That difference is critical.
She noted that the ER is built to rule out what could cause serious harm in the short term—not what may be causing long-term pain and disruption. As a result, patients with endometriosis often leave the ER without answers, even when their pain is severe and persistent.
Why this matters:
- Normal scans or lab results don’t mean your pain isn’t real.
- Endometriosis is often invisible to standard imaging and labs used in emergency care.
- ER visits should be followed by an evaluation from a provider who specializes in endometriosis.
Key takeaway: Emergency rooms are for short-term safety. Long-term answers come from specialist care.
2. Endometriosis mimics many conditions, which contributes to delays in diagnosis
Dr. Sbiroli described endometriosis as “the great mimicker,” noting that its symptoms can resemble everything from appendicitis to urinary tract infections to irritable bowel syndrome. This makes diagnosis particularly challenging—especially when patients present with pelvic pain that overlaps with multiple other conditions.
For patients, this means:
- You may receive a different diagnosis—sometimes several—before endo is even considered.
- ER providers must rule out dozens of possibilities before settling on a non-emergency cause.
- Clearly describing what feels different about a particular episode can help guide evaluation.
Key takeaway: Tracking your symptoms and using specific language can help avoid misdiagnosis and guide the next steps.
Video: Endometriosis Misdiagnosed in the ER
3. Endometriomas are different from other cysts—and ruptures can make endo worse
Unlike functional cysts, which typically resolve without intervention, endometriomas are associated with endometriosis and contain inflammatory tissue. Dr. Goldstein explained that when endometriomas rupture, the fluid can spread throughout the pelvis, potentially seeding more disease and leading to further complications.
If possible, endometriomas should be removed in a controlled surgical setting—not left to rupture.
Signs that suggest a rupture may have occurred:
- Sudden, sharp, localized pain (often on one side)
- Onset after physical activity, sex, or ovulation
- Nausea, dizziness, vomiting, or abdominal swelling
Key Takeaway: A ruptured endometrioma is a serious condition—not a benign event. If your pain is sharp, sudden, or feels distinctly different from your usual symptoms, seek care immediately and follow up with a specialist.
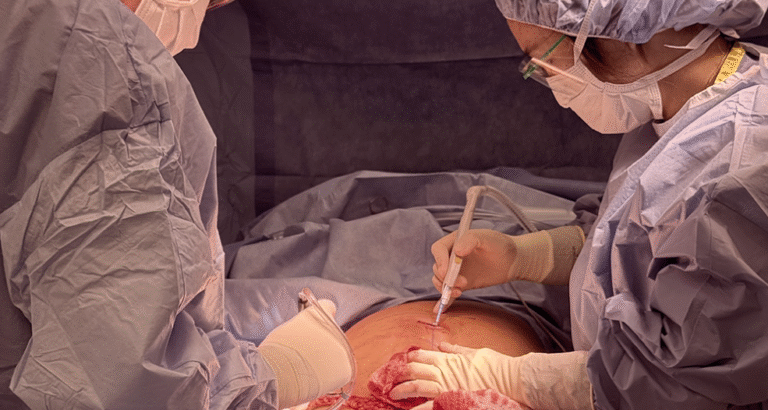
An experienced endometriosis specialist should perform emergency surgery. We cannot emphasize this enough. When endometrioma surgery is done by someone unfamiliar with the nuances of endometriosis care, it can lead to complications—including the unnecessary removal of an ovary.
If you suspect you have a large endometrioma and need support on a more urgent timeline, please don’t hesitate to call our office. We’re here to help guide you safely and expertly.
4. MRIs for endometriosis require expertise and appropriate timing
Although MRIs can sometimes detect deep infiltrating endometriosis, Dr. Goldstein emphasized that this type of imaging is not typically performed in the emergency room. When it is done, it may be read by general radiologists who do not routinely look for endo-specific pathology.
She recommends scheduling MRIs through a specialist’s office, where the imaging is performed using appropriate protocols and reviewed by radiologists trained to identify endo.
What patients should know:
- Emergency rooms rarely offer pelvic MRIs for non-life-threatening conditions.
- Even when MRIs are performed, their usefulness depends on who reads them.
- Outpatient imaging arranged by an endo-informed provider is more likely to yield meaningful results.
Key takeaway: The right imaging, done by the right team, can make a real difference. It’s worth waiting for the correct setting.
Video: Why You Usually Can’t Get an MRI for Endometriosis in the ER
5. Some endometriosis-related symptoms are emergencies—know when to go
Although most flares are not life-threatening, endometriosis can affect other organs in ways that do require emergency care. Dr. Goldstein outlined several examples, including obstruction of the kidneys (hydronephrosis), thoracic endometriosis causing chest pain or lung collapse, and bowel-related complications such as obstruction or severe GI distress.
Symptoms that may require immediate care:
- Pain that causes fainting, vomiting, or difficulty walking
- Severe bloating, inability to pass stool or urinary retention
- Chest pain or shortness of breath
- Heavy bleeding that soaks a pad in under an hour
Key takeaway: Not all pain is an emergency—but when symptoms escalate, it’s important to go to the ER and follow up with your care team.
Helpful tip: Always ask for a copy of any imaging performed (on a disk), as well as your labs and emergency room records. These provide a crucial snapshot of what was happening at that moment. If possible, also note which day of your menstrual cycle you were on—whether around ovulation, pre-period or during your period—as this context can be very informative.
Bringing It All Together
This conversation shed light on the fundamental gaps in care many patients experience when living with endometriosis—and how better information, planning, and support can help. ER visits can be confusing, even disheartening when you’re told, “Everything looks fine.” What they may mean to say is this is not an immediately life-threatening condition- and you can seek care long term from a specialist focused on endometriosis. We understand these trips are tough and disheartening. But with the right tools, expectations of what an ER can do for you and appropriate follow-up they can also be an important part of your journey toward answers.
At ESSE Care, we help patients:
- Track symptoms and recognize red flags
- Advocate effectively in urgent care settings
- Access expert surgical care and thoughtful follow-up
- Build a supportive, integrative plan for long-term healing
You are not overreacting. Your pain is not invisible. You deserve to be heard, believed, and supported.