To honor four years since her life-saving endometriosis excision surgery, Lisa Lisiewski—stage IV endometriosis survivor and functional nutritionist—joined Dr. Karli Provost Goldstein for a conversation about what really happens after surgery.
Lisa’s story is more than a recovery story—it’s a guidepost for what patients should know about life after endometriosis excision. Together, Lisa and Dr. Goldstein explored what healing requires in the months and years following surgery and how intentional, integrative care can change the outcome.
Here are the top five takeaways from their conversation—offering both hope and guidance for anyone navigating the path beyond surgery.
Top 5 Insights from Lisa’s Healing Journey Four Years After Endometriosis Surgery
1. Endometriosis symptoms aren’t always what you expect.
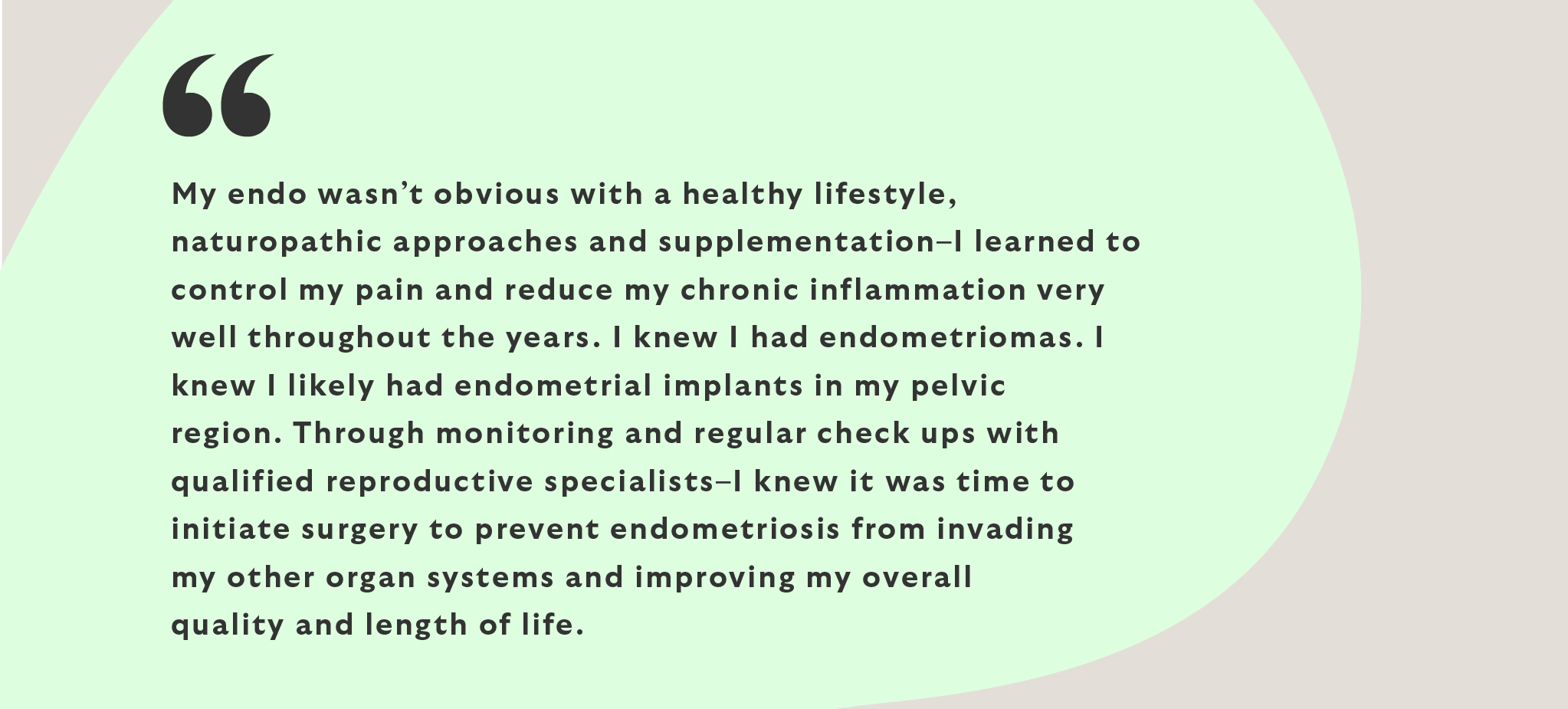
Lisa had stage IV disease with bowel, renal and diaphragm involvement—but she wasn’t doubled over in pain. She was working 70 hours a week, running her practice, and managing symptoms with nutrition, supplementation and movement.
You can have advanced disease without classic endometriosis symptoms. That’s why:
- GI symptoms like bloating, loose stools, or constipation shouldn’t be dismissed.
- Cyclic fatigue, brain fog, chronic pelvic pain or ovulation pain may indicate deeper issues.
- Not every patient presents with debilitating period pain—but many still need surgery.
2. Surgery isn’t the finish line—it’s the beginning of a new phase of care.
Expert excision surgery can be life-changing. It removes disease, restores anatomy, and relieves pressure on critical organs. But surgery alone isn’t a cure. Endometriosis is chronic, systemic, and often layered with other conditions like adenomyosis.
After surgery, patients should expect to focus on:
- Inflammation control through nutrition, movement, and gut health
- Hormonal balance, especially after surgical menopause or ovarian conservation
- Tissue and scar healing through pelvic floor therapy and physical rehab
- Surveillance and lab monitoring to watch for recurrence or new concerns

3. Post-operative recovery is multidimensional.
Lisa’s recovery included surgical menopause, a temporary colostomy, and emotional trauma from years of misdiagnosis. She also lost an aunt to similar complications—and carried the emotional weight of that experience.
Post-op healing often requires:
- Emotional support or trauma therapy
- HRT to manage sleep, mood, cardiac, neurological and bone protection
- Pelvic floor therapy to restore mobility and function
- Nutritional support and GI healing from bowel surgery or years of gut dysfunction
- Community and connection to process the experience and feel seen
4. Lifelong care doesn’t mean constant crisis—it means intentional maintenance.
Many patients worry that if endometriosis can come back, they’ll never feel safe or stable. But Lisa’s story shows that with consistent support, the body can thrive.
She no longer lives in fear of her disease. Instead, she lives in partnership with her care—adjusting when needed, checking in regularly, and staying proactive.
Lifelong care for endometriosis may look like:
- Annual (or biannual) labs for hormones, inflammation, lipids, and nutritional markers
- Bone density scans (DEXA) after menopause
- Hormone replacement therapy (HRT) tailored to your stage of life and symptoms
- GI and pelvic therapy to manage surgical changes or digestive shifts
- Continued nutrition and supplement support to reduce symptoms and inflammation response
5. You can feel incredible—even if endometriosis isn’t completely gone—with the right support.
At four years post-op, Lisa feels strong, energized, and deeply well. There may still be microscopic disease present—but it isn’t active, and she isn’t symptomatic. This is the realistic hope we want patients to know: you may still live with endo, but you don’t have to suffer from it.
Her care now includes:
- Strength training and movement
- Anti-inflammatory nutrition and GI care
- Supplements to support hormone and immune health
- HRT customized to her body’s needs
- Regular check-ins and labs to track changes
What to Expect After Your Endometriosis Surgery: A Snapshot
Here’s an example of what a post-op care plan could look like at ESSE Care. This is a high-level, non-medical overview intended to provide general guidance. Each plan is individually tailored based on your body, recovery needs, and surgical findings. The timeline shown here is only a reference—your specific care will depend on the extent and complexity of your case.
|
Timeline |
What to Expect |
|
0–3 months |
Surgical recovery, HRT within seven days, hormone lab monitoring and adjustments, pain management, and bowel support. Walking and light exercise may begin in 4–6 weeks if cleared. Avoid heavy lifting for 6–8 weeks. Typical return to work is 2–4 weeks. |
|
3–6 months |
Begin pelvic floor PT; post-op ultrasound at 3 months (or cuff check for hysterectomy); optimize nutrition; start HRT if needed |
|
6–12 months |
Labs, bone scan (if menopausal), symptom tracking, begin deeper fitness or GI goals |
|
Year 1–2 |
Maintenance labs, continued PT/nutrition, surveillance imaging (if symptoms warrant) |
|
Year 3–5+ |
Lifelong monitoring, HRT updates, GI/pelvic refreshers, fitness goals, integrative therapies |
At ESSE, You’re Not Alone After Surgery—We Stay with You
Lisa’s story reminds us that healing isn’t a one-time event—it’s a long-term, empowering process. At ESSE Care, we’re committed to walking that path with you, offering expert surgical care and the integrative support that sustains your wellness for years to come.
Whether you’re recovering from recent excision surgery or wondering what’s next in your endometriosis care, we’re here—with knowledge, compassion, and a whole-body approach. If you need support, reach out to our team today.