For most patients, gynecologic surgery isn’t about cosmetic change or convenience—it’s about reclaiming their health. For those living with advanced uterine conditions like fibroids and endometriosis, the physical toll can be profound: chronic pain, relentless bleeding, and a life constantly interrupted. At ESSE Care, our goal is to restore both health and dignity to patients who’ve often been misdiagnosed, dismissed, or left in limbo for years.
This patient’s story is one example of why comprehensive, compassionate care—and skilled surgery—can be life-changing.
About Uterine Fibroids and Endometriosis
Two of the most common—but often misunderstood—gynecologic conditions are uterine fibroids and endometriosis. While they can occur separately, many patients, like the one in this case, experience both at once, which can intensify symptoms and complicate treatment.
Uterine Fibroids (Leiomyomas)
- Non-cancerous growths that develop in or on the uterus.
- Can cause heavy menstrual bleeding, pelvic pain, bloating, and pressure symptoms.
- When large or numerous, they may distort the uterine cavity and lead to complications like increased blood loss each period, long-term iron deficiency anemia, and pregnancy complications.
- Extremely common—up to 80% of women have fibroids by age 50.
- Many cases don’t cause pain or other obvious symptoms, but even “asymptomatic” fibroids can require surgical treatment due to severe anemia.
Endometriosis
- A chronic inflammatory condition where tissue that looks similar to the inner uterine lining (when viewed under the microscope) grows outside the uterus in multiple places throughout the body.
- It can lead to severe pelvic pain, especially during menstruation, and is a leading cause of infertility.
- In some patients they may not have painful periods but have extreme bloating, constipation, diarrhea, nausea, and bowel symptoms.
- Endometriomas, or “chocolate cysts,” can create dense scar tissue.
- It can cause adhesive disease where organs can bind together, causing a “frozen pelvis” that makes surgery more complex.
Patient Case Summary: A Body Under Siege


The patient had been living with massive uterine fibroids and advanced-stage endometriosis. These conditions led to chronic blood loss anemia so severe that she required multiple blood transfusions over time. Her symptoms were debilitating, and not just physically. The constant bleeding and exhaustion had eroded her quality of life. She experienced shortness of breath when climbing stairs and headaches from loss of blood to her brain. Chronic low energy made her want to cancel plans or not show up to work. She was offered hormone treatment for many years, but the fibroids continued to grow.
While many patients are initially offered hormonal treatments or told to “watch and wait,” this patient’s case was far beyond conservative management. She needed surgery not just to treat pain or improve function but to stop the damage being done to her body. At severe levels, chronic blood loss anemia eventually causes loss of blood to the most vital organs in your body (heart, brain, kidneys, liver, etc.).
Diagnosis and Pre-Op: A Surgical Plan with Purpose
Dr. Goldstein took a careful and thorough approach to this case. The surgical plan included:
- An open hysterectomy to remove the uterus.
- A transparent discussion about the long-term implications of having a massive fibroid uterus shaped like a pregnancy belly.
- A collaborative approach with a plastic surgeon, who recommended a low transverse bikini line incision and vertical inner incisions to remove the fibroid uterus. Despite numerous surgical consultations with other doctors, this was the first time the patient was offered a horizontal incision rather than a large midline incision, which is difficult to disguise even after it heals.
- An abdominoplasty (commonly referred to as a tummy tuck) to address excess abdominal skin. After decades of stretching due to inflammation, bloating, and body changes, the skin’s elasticity was damaged and was unlikely to bounce back after surgery. The plastic surgeon examined her abdomen and recommended removal of all excess skin.
The goal was to help her heal fully, both inside and out, by feeling confident about her choices and empowered to get her body back!
Inside the OR: Uncovering the Full Picture
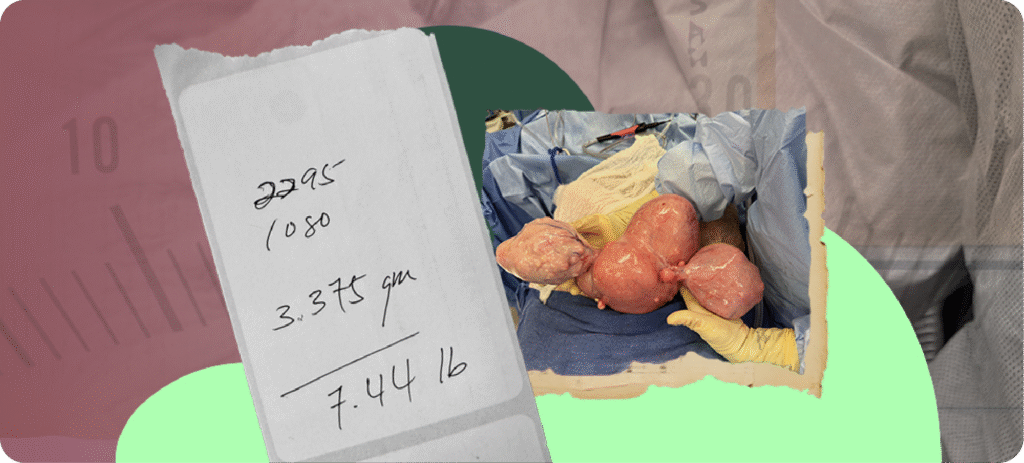
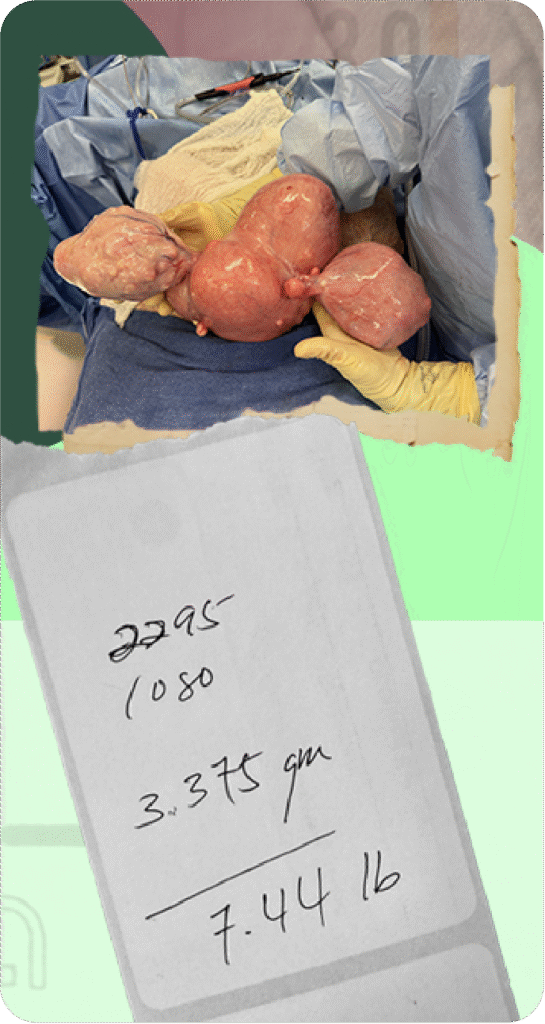
Once in surgery, the complexity of the case became clear. The uterus was enlarged and distorted by fibroids, as expected. But more striking was what lay behind it: endometriomas had developed on both ovaries, and the ovaries themselves were fused to the uterus by dense scar tissue. One of the most shocking facts of this case is just how large and heavy the patient’s organs had become. A normal, healthy uterus and ovaries weigh just 2-3 ounces; when the surgeons put the patient’s extracted organs on the scale, they weighed in at a whopping 7.44 lbs. after all the blood had drained out of them. The surgeon stated prior to weighing and draining the uterus, it felt like 20 lbs.!
While the surgical team was prepared for challenges, the extent of the disease underscored the importance of timely intervention. This kind of “frozen pelvis” is a hallmark of advanced endometriosis, and it takes careful surgical technique to separate organs safely. Dr. Goldstein meticulously dissected the adhesions, removed the uterus and ovaries, and worked with a bowel surgeon and a urologist to address the bowel and ureters. (Due to advanced endometriosis, the right kidney outlet and ureter had been compromised and required a prophylactic ureter stent for several weeks after surgery.) Finally, Dr. Goldstein partnered with an expert plastic surgery team who completed the abdominoplasty.
What to Expect After an Open Hysterectomy
Recovery from an open hysterectomy takes time, but for patients living with severe gynecologic disease, the benefits are often transformative. Here’s what you can expect:
- Hospital stay: Up to a few days of inpatient recovery to monitor healing and pain control
- Initial healing: Rest and limited activity for several weeks, with gradual return to normal routines. Walking initially is recommended multiple times a day with gradual return to exercise after 6 weeks.
- Pain management: Medications and supportive care to manage post-operative discomfort
- Hormonal changes: If ovaries are removed, some patients may experience menopausal symptoms. Hormonal therapy can help.
- Abdominoplasty: Requires use of drains to reduce swelling and fluid accumulation after surgery as well as special body positioning to keep legs elevated and chest forward. Drains require care at home and in-office removal two weeks after the initial operation.
For patients like this one, who had large fibroids, chronic blood loss, and advanced endometriosis, the most noticeable change often comes in the form of relief. Without a uterus producing constant bleeding or ovaries driving disease progression, many patients experience a dramatic drop in fatigue over time, pain, and inflammation. They can finally move, breathe, and live without the persistent drag of pelvic disease.
While full healing can take several months, many report a sense of lightness—both physically and mentally—as their bodies recover. No more monthly bleeding. No more transfusions. No more planning life around pain. This surgery isn’t easy, but for those who need it, it can be the start of a new chapter.
Why This Matters
Too often, people with complex gynecologic conditions are told to “wait and see” or that surgery is extreme, even when their bodies are screaming for help. Symptoms like heavy bleeding, pelvic pressure, fatigue, and pain are normalized or minimized, leading to delayed diagnoses and avoidable complications. That delay can come at a steep cost: chronic blood loss, transfusions, and organs physically fused together by scar tissue. For this ESSE Care patient, a surgical solution was not only appropriate—it was essential.
Here are the key takeaways from this case:
- Fibroids can cause serious complications, including anemia. When large or numerous, fibroids can lead to heavy bleeding and iron deficiency that may require transfusions if left untreated.
- Endometriosis doesn’t just cause pain—it causes damage. Advanced-stage endometriosis can spread, create adhesions, and lead to “frozen pelvis,” where organs are stuck together and surgery becomes more complex.
- Expert surgical care makes a difference. Knowing what to look for, how to prepare, and how to manage complex anatomy in the OR is critical for safe, effective outcomes.
At ESSE Care, we want patients to know: your symptoms are valid. If you’re bleeding heavily every month, feeling wiped out, or dealing with unexplained pelvic pain, speak up. Ask about imaging. Ask for second opinions. The right diagnosis changes everything.
Dr. G’s Final Thoughts
“People often think of hysterectomy as the end of something—but for so many patients, it’s the beginning. Once the disease is gone, you finally have space to heal. This patient had been through so much, and it was an honor to give her relief and a cosmetic appearance on the outside as beautiful as the newly restored pelvis is on the inside. This allowed her to feel comfortable with the decision to remove her uterus but also gain something beautiful she wanted at the same time.” – Dr. Karli Provost Goldstein
At ESSE Care, we believe every patient deserves to feel heard, respected, and fully treated. If you’re living with complex gynecologic disease, know that there is a path forward.
Ready to talk to our surgical team? Contact us today for a case review and discover more about our patient-centered approach.












