If you’ve been experiencing chronic pain, digestive issues, or unexplained infertility, but doctors keep dismissing your concerns, you’re not alone. Many people with endometriosis struggle for years before receiving a proper diagnosis. The reality is that endometriosis is often overlooked, misunderstood, and downplayed, leaving patients to suffer in silence.
The Truth About Endometriosis
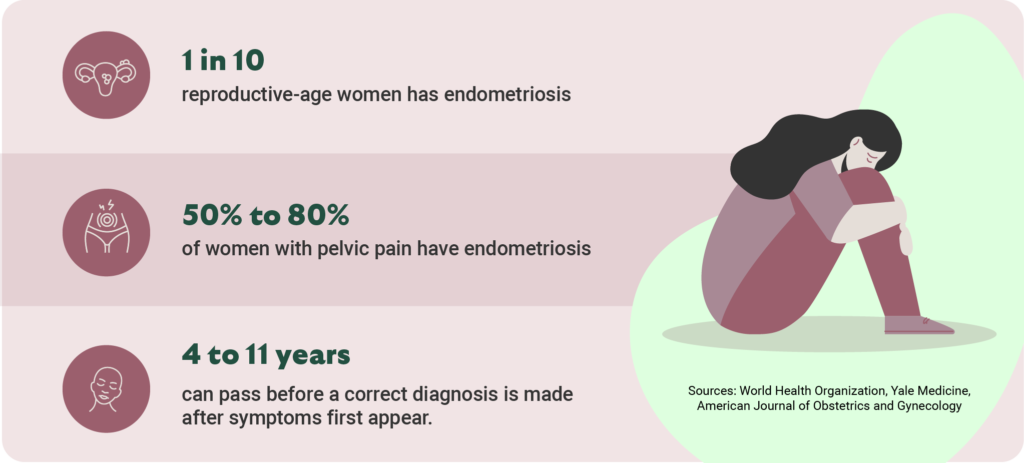
Endometriosis is more than just “bad periods.” It’s a condition where tissue similar to the uterine lining grows outside the uterus, causing inflammation, pain, and sometimes severe organ involvement. Despite affecting around 1 in 10 reproductive-age people assigned female at birth and 50% to 80% of women with pelvic pain, it remains notoriously underdiagnosed.
Many patients are told their pain is “normal” or “just part of being a woman.” This medical gaslighting leads to delayed diagnoses and years of unnecessary suffering. But endometriosis is a progressive disease—meaning early diagnosis and treatment are critical.
Endo Symptoms Go Beyond Period Pain
Video: True or False: Endo Only Causes Painful Periods
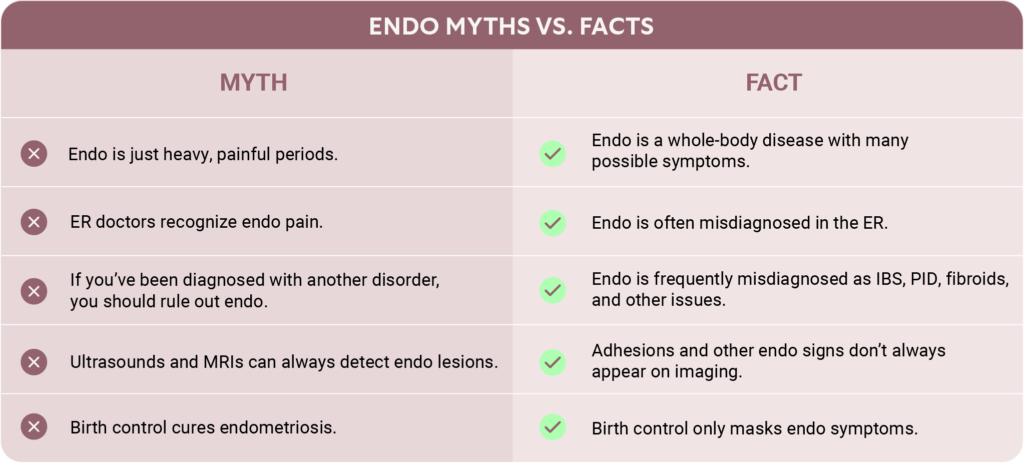
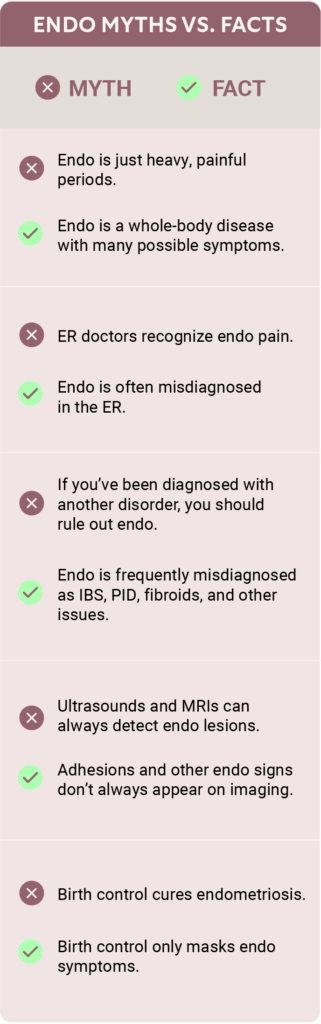
There are several misconceptions about endometriosis and periods:
- Endometriosis only causes painful periods.
- Women who don’t have painful periods must not have endometriosis.
- Endometriosis always causes heavy periods.
The truth? Some patients may have light or manageable periods with very little pain but experience other problems like recurrent miscarriage or bowel symptoms. Symptoms depend on where the endometriosis lesions grow. Plus, some cases of endometriosis don’t result in any symptoms at all until a woman tries (and fails) to conceive.
Endometriosis doesn’t just affect the reproductive system—it can grow in other areas of the body as well. Some patients develop endometriosis on the bowels, bladder, or even in distant organs like the diaphragm and lungs. This can lead to symptoms like chest pain, shortness of breath, shoulder pain, or, in rare and severe cases, coughing up blood during your menstrual cycle. Because these symptoms seem unrelated to gynecological issues, they are often overlooked.
So, you could have endometriosis and never experience severe cramps. Instead, you might have:
- Chronic pelvic pain that doesn’t follow a clear pattern
- Pain during or after sex
- Bladder issues, such as frequent urination or a constant feeling of pressure
- Severe digestive problems, including bloating, constipation, diarrhea, or small intestinal bacterial overgrowth (SIBO)
- Back, chest, or even shoulder pain
- Unexplained infertility
If your symptoms worsen around your menstrual cycle, that’s a major red flag—but not all doctors will recognize it.

ER Doctors Often Misdiagnose Endometriosis
Emergency rooms frequently misdiagnose endometriosis-related pain. Patients experiencing severe bladder pressure, chest pain, or lower back pain may be sent home with generic pain relief and incorrect diagnoses, such as urinary tract infections (UTIs) or muscle strain.
Patients are frequently told in the ER they have “cyst rupture” or that ovulation is causing their pain.
For example, one case involved a patient repeatedly visiting the ER for lower back pain and urinary symptoms. She was given handouts for back exercises and dismissed. Weeks later, a laparoscopy confirmed she had extensive endometriosis, including large ovarian cysts known as endometriomas.
Had doctors asked the right questions—such as whether her symptoms correlated with her menstrual cycle—she might have received proper care sooner.
Misdiagnosis Can Cause Years of Pain
While it’s impossible to know exactly how often endometriosis is misdiagnosed as another condition, we do know that these incorrect diagnoses frequently lead to years of unnecessary suffering for women ultimately diagnosed with endo. Research shows that for many patients, the journey to a definitive endometriosis diagnosis can take anywhere from 4 to 11 years after their symptoms first appear. Depending on the symptoms patients exhibit, misdiagnoses can include everything from irritable bowel syndrome (IBS) and pelvic inflammatory disease (PID) to uterine fibroids, interstitial cystitis, and even anxiety.
You know your body, and doctors should trust their patients when they say something is wrong. If you’ve received treatment for a different disorder or disease but are still experiencing symptoms related to endometriosis, consider seeing a specialist.
Imaging May Fail to Detect Endometriosis
Video: Do Adhesions Always Show Up on Imaging?
Many doctors rely on ultrasounds or MRIs to rule out endometriosis, but these tests aren’t always effective. In particular, adhesions—bands of scar tissue, caused by endometriosis, that bind organs together—often don’t appear on imaging. And doctors without training or experience diagnosing endometriosis may not know what to look for. Clues that an endo specialist might notice during imaging include fluid collections in pockets of the organs, peritoneal inclusion cysts, or filmy lines that shift with pressure or probing.
If a doctor dismisses your symptoms because an ultrasound came back “normal,” don’t accept that as the final answer. Adhesions can lead to severe pain and dysfunction and may develop due to pelvic surgery, infections, or even IVF egg retrievals. Symptoms can include:
- A pulling sensation in the abdomen
- Bladder pressure or difficulty emptying your bladder completely
- Persistent digestive issues
If you have a history of pelvic surgeries or infections, it’s crucial to consider adhesions as a potential source of pain. The only definitive way to diagnose endometriosis is with minimally invasive laparoscopic or robotic surgery where a surgeon carefully examines the abdominal and pelvic region for lesions, but a well-trained specialist may be able to notice the right signs before you decide on surgery.
Birth Control Can Mask Endo Symptoms
Some doctors prescribe birth control as a “solution” for endometriosis. While hormonal birth control can help manage symptoms, it does not stop the disease from progressing. Patients can be on birth control for decades, only to discover they have Stage IV (severe) endometriosis when they try to conceive.
One ESSE Care patient had been on birth control for 20 years, only to learn that her endometriosis had caused severe organ damage, complicating her ability to preserve fertility. If your doctor dismisses your symptoms because “birth control should be helping,” push for further evaluation.
How to Advocate for Yourself
If you suspect you have endometriosis, don’t wait for a doctor to take your pain seriously. Here’s what you can do:
- Track your symptoms—particularly, note patterns related to your menstrual cycle. Do certain problems get worse right before or during your period?
- Request a referral to a specialist (not just an OB-GYN, but an endometriosis excision specialist).
- Push for further testing, including laparoscopy, if symptoms persist.
- Seek a second (or third) opinion if your concerns are dismissed.
At ESSE Care, we believe your pain is real, and your concerns matter. If you’ve been told your symptoms are all in your head or that your pain can’t be treated, know that you deserve better care. We’re here to help you get the answers and relief you need.
Book a case review today and let our endometriosis experts answer all your questions.












