A Collaborative Conversation with ESSE, CCRM, and Trusted Partners
The IVF vs. Endometriosis Surgery webinar, hosted by Dr. Karli Provost Goldstein, brought together an expert panel including Dr. Sheeva Talebian (Reproductive Endocrinologist at CCRM New York), Dr. Mary Sabo (Acupuncturist and Integrative Hormone Specialist at LILY + HORN), and Dana (Patient Advocate and IVF graduate), for a deeply honest, clinically grounded discussion about fertility, surgery, and what happens when the full body isn’t factored into care.
Together, they explored how collaborative, sequenced, and whole-person planning can transform outcomes—and offer hope to patients navigating complex, often overwhelming fertility journeys.
Here are the top five takeaways from the conversation:
1. Endometriosis can silently interfere with fertility—even when imaging looks “normal”
Dr. Goldstein emphasized that endometriosis is not just a disease of pain—it’s a disease of inflammation and disruption, often invisible to labs or ultrasounds.
Even when patients don’t have severe symptoms, endometriosis can impact:
- Egg quality
- Ovulation
- Tubal function
- Uterine receptivity
Many patients—like Dana—have normal imaging, “mild” symptoms, and still face repeated IVF failure. This is why surgical evaluation matters, especially when outcomes don’t match expectations.
2. IVF is powerful—but it works best when the body is ready
Dr. Talebian shared how IVF remains a critical tool for many families—but it’s not magic. If endometriosis is creating a hostile environment inside the pelvis or uterus, no amount of stimulation or protocol adjustments will fix the core issue.
That’s why strategic sequencing is key:
- Sometimes IVF should come first.
- Sometimes surgery is the right next step.
But always—it should be a collaborative decision, based on full-body context and your unique timeline.
3. Surgery can be a reset—not a last resort
Dana’s story reminded us that excision surgery is not a failure of IVF—it’s a turning point in understanding what your body really needs.
Her journey included three IVF cycles, declining embryo quality, and rising anxiety. After excision, not only did her embryo outcomes improve—but she gained confidence and clarity. She was no longer guessing.
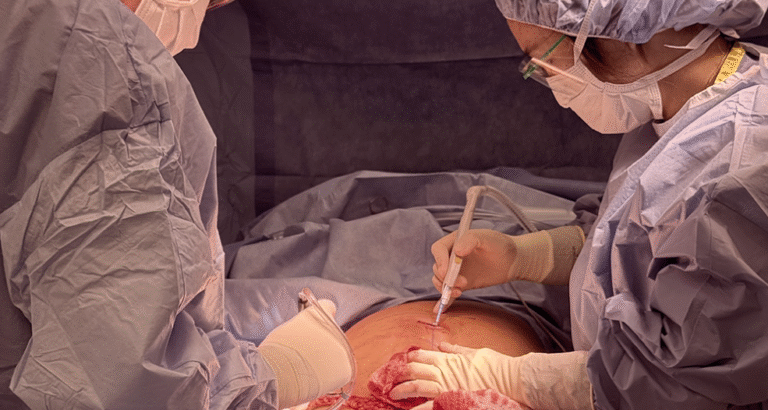
Dr. Goldstein explained that surgical excision removes active lesions, restores anatomy, and gives you a clean slate—whether you’re trying naturally or moving forward with ART.
4. Whole-body care strengthens fertility at every stage
Dr. Sabo shared how acupuncture, nervous system regulation, and hormone optimization support every step of the fertility journey—before IVF, after surgery, and through recovery. She highlighted the power of:
- Improving ovarian response with cycle-specific acupuncture
- Supporting hormone clearance and digestion post-surgery
- Calming cortisol and stress for better reproductive function
Dana credited her acupuncture care with helping her feel more grounded and less reactive during the highs and lows of IVF. This kind of integrative care isn’t alternative—it’s essential.
5. The future of fertility care is collaborative—not siloed
What made this conversation powerful wasn’t just the insight from each speaker—it was how their voices aligned. Each specialist brought a different lens, but the same philosophy: The patient comes first. The whole body matters. And healing happens best in partnership.
At ESSE, this is our model:
- Surgery when it’s needed.
- IVF when it’s most likely to succeed.
- Acupuncture, nutrition, and nervous system care all along the way.
No guessing. No gaps. No shame. Just a team walking with you.
Moving the Conversation Forward
Patients navigating endometriosis and infertility don’t need more pressure—they need more clarity, more support, and more options that make sense.
At ESSE, we’re building care around you:
- Your body.
- Your timeline.
- Your values.